Fish Oil (EPA+DHA) Rocks, but Promote Kidney Stones, Cancer, and Obesity (With Fructose); Unsat. Vegetable Oil, and Wheat Are Bad
source: http://perfecthealthdiet.com/?p=1177
You need DHA in your diet (EPA can be synthesized from ALA, which is in flaxseed oil; DHA barely can). But high levels of polyunsaturated fats may be dangerous; they’re easily oxidized (anecdotal evidence; natural diets don’t have high levels, unless they’re mostly fish): You can supplement DHA from some particular type of seaweed (I forget the details), or in many fatty fish or their extracted oil (watch your mercury). It does occur naturally in lesser quantities in various other foods. DHA lowers testosterone, but it has many good effects. Lower testosterone means more (harmless, operable) prostate cancer, but possibly more frequent severe cases:if DHA is dangerous, low-fat dieters will be in the most trouble. Another reason to eat a high-fat diet.
(the ratio matters; eat more saturated fat to mitigate the harms while still getting some of the benefits of DHA)
Most Americans eat far too much omega-6, and their omega-6 to omega-3 tissue ratio is too high, which is pro-inflammatory via the COX-2 pathway. Eating omega-3s including DHA reduces inflammation by downregulating the COX-2 pathway. This accounts for the well-attested benefits of DHA against cardiovascular disease. Now, cancer is promoted by COX-2 pathway inflammation, which is why COX-2 inhibitors such as aspirin and ibuprofen are protective against cancer. [4] DHA’s action to downregulate this pathway must generate an anti-cancer effect. But, unlike aspirin and ibuprofen, DHA has no observable effect on overall cancer risk. This suggests that DHA has other effects, unrelated to its anti-inflammatory activity, that are cancer promoting. These counterbalance the benefits from its anti-inflammatory effect. If DHA has pro-angiogenic effects that are independent of COX-2 mediated inflammation, then this could account for the observations.
One reason an association of DHA with high-grade cancer may have been missed is that it would be detected only in large studies able to segregate cancers by grade.
a person in whom the immune system is trying but failing to clear elevated CEP levels almost invariably has macular degeneration (AMD)
AMD = why 1/3 of people 75+ yr old are nearly blind. DHA is the only cause of CEP. It’s caused by excessive growth of blood vessels dislodging the retina. DHA is concentrated near the retina (is 80% of the PUFA in it). Photons cause oxidation, and DHA is extremely oxidizable. Antioxidants help slow AMD. Finally, adding CEP directly to mice causes AMD (this was shown in 2003). (we know now it’s because CEP causes angiogensis).
CEP is normally good. It brings immune cells from bone marrow to the wound. Cancers and AMD give chronic CEP elevation. CEP actually causes wound healing even in mice with normal wound healing mechanisms crippled (VEGF and TLR2 knocked-out or inhibited) - this was shown in 2010. VEGF causes angiogenesis when tissue is oxygen deprived. TLR2 causes angiogenesis when it detects oxidative stress. vitamin A + DHA yield CEP (via retinyl from A + HOHA=oxidized DHA). If you’re going to take DHA (usually fish oil) you’ll want anti-oxidants. Oxidation can’t be avoided; it’s essential to metabolism and fighting infection.At the moment, I think it’s prudent to eat no more than 1 pound of salmon or similar cold-water fish per week, to avoid further EPA/DHA supplements, and to avoid low-fat diets which tend to elevate membrane DHA levels. Moderate omega-3 consumption is especially important for those suffering from diseases of pathological angiogenesis – especially cancer. DHA is essential for good health – but in excess, it is probably dangerous.
ouch.
DHA + retinyl + oxidative stress = angiogenesisThis recipe is invoked normally and properly during wound healing. But it is also invoked excessively in pathological contexts – notably in cancers and age-related macular degeneration, probably also in other angiogenesis-associated diseases such as arthritis, rosacea, obesity, psoriasis, endometriosis, dementia, and multiple sclerosis.
Finasteride raises DHA levels, and DHA lowers testosterone. Low testosterone reduces incidence of low-grade prostate cancers but makes it much more likely they will progress to high-grade. Thus, finasteride reduces prostate cancer incidence but increases high-grade prostate cancer incidence and overall prostate cancer mortality. Fits all the facts. Could be.
source: http://perfecthealthdiet.com/?cat=27
My bottom line: the Brasky study is weak evidence for anything, but it does raise a whiff of evidence that high dietary fish oil intake might encourage a transition from low-grade to high-grade cancer.
Lycopene may be the most powerful carotenoid quencher of singlet oxygen,[18] being 100 times more efficient in test tube studies of singlet-oxygen quenching action thanvitamin E … The absence of the beta-ionone ring structure for lycopene increases its antioxidant action….
Lycopene is not modified to vitamin A in the body …
So lycopene does not increase retinyl levels, but does act as an extraordinarily powerful antioxidant, thus reducing oxidative stress! If you wanted a good food for stopping the DHA – angiogenesis pathway, you’ve found it: tomatoes.
Eat tomatoes. (the other carotenoids mostly can convert to vit A, and overly high levels of vit A mean slightly higher risk of aggressive cancer).
Prostate cancer is associated with low tissue levels of zinc. [7, 8] High dietary intake of zinc is associated with lower rates of prostate cancer. [9]
N-acetylcysteine is an antioxidant supplement that is a precursor to glutathione. N-acetylcysteine has been shown to prevent angiogenesis and has been proposed as a likely cancer preventative, but this is as yet untested. [10]
Observational studies weakly link high DHA, high vitamin A, and low antioxidant status to diseases of angiogenesis such as cancer.
This pattern would be consistent with the idea that the natural pathway used in wound healing to trigger angiogenesis – DHA oxidation and combination with retinyl protein to trigger TLR-2 pathways – is also important for cancer progression.
It suggests a strategy of reduced fish oil and vitamin A consumption and increased intake of certain antioxidants (such as lycopene, zinc, selenium, or NAC) may be helpful against cancer.
However, this idea needs testing. No study in animal cancer models has tested this dietary combination.
Given the many proven benefits of moderate amounts of fish oil, I don’t see a reason yet to alter our recommendation that healthy people should eat a pound of fish per week. That said, I do think very high intakes of fish or fish oil are ill advised. And I’m intrigued by the idea that dietary changes may have the potential to play a powerful role in recovery from diseases of angiogenesis such as cancer.
A few years ago I started taking a high dose of Omega 3, because of joint inflammation, and other issues. This made big difference for about 3 months, then seemed to not work any more. I talked to a nutritionist friend and she pointed out that according to Andrew Stoll (The Omega 3 Connection) you must take 1000 mg vit C and 500 iu vit E daily or the omega 3 becomes oxidised in your body (cell membranes) and ineffective. I started taking both and in days was back to the original anti-inflammatory effectiveness of omega 3. I have since talked to others about this – for example a psychiatrist whose clients did well on omega 3 for 3 months and then it became ineffective.
quite anecdotal - needs actual research. but the fact that omega-3 are easily oxidized means they might degrade vit-C (which means you need enough carbs+selenium in your diet to move the DHAA out of the bloodstream into cells for reconversion to C, or you just need to bear the harm of DHAA and supplement more C. In general, vit E supplementation is quite harmful. I wouldn’t do it unless strong evidence revealed that it’s okay when you have high omega-3 intake.
Vitamin C deficiency tends to develop slowly over months, losing a little every day, so it’s quite plausible that a deficiency could develop over 3 months and lead to those changes in omega-3 oxidation.
It is possible that extra lipid peroxidation on a high-PUFA diet could help deplete vitamin C faster.
data seem to show that people taking particularly high doses of vitamin E (500 IU to 2000 IU) may have a slightly increased risk of death. However, taking 400 IU vitamin E per day did not increase the risk of death in a total of 15,000 patients studied in several different clinical trials.
source: http://www.nei.nih.gov/news/statements/vitamine.asp
Eating omega-3 fats promotes calcium oxalate kidney stones about as much as eating oxalate. The top quintile of dietary oxalate intake has a relative risk of 1.22. [12] (The top dietary source of oxalate is spinach, by the way.)
a reminder from my last post:
Zero-carb dieters are at risk for
- Excess renal oxalate from failure to recycle vitamin C;
- Excess renal uric acid from disposal of nitrogen products of gluconeogenesis and ketogenesis;
- Salt and other electrolyte deficiencies from excretion of oxalate, urea and uric acid; and
- Dehydration.
If you feed lab animals high doses of polyunsaturated fat (either omega-6 or omega-3 will do) along with high doses of either fructose or alcohol, then fatty liver disease develops along with metabolic syndrome. Metabolic syndrome is a major risk factor for obesity, and it’s not very difficult to induce obesity on these diets.
source: http://perfecthealthdiet.com/?p=1963
Both sugar and vegetable oils are individually risks for obesity:
- Stephan did a nice post a few years back, “Vegetable Oil and Weight Gain,” discussing a couple of studies showing that both rats and humans get fatter the more polyunsaturated fat they eat.
- Dr. Richard Johnson and colleagues did a review of the evidence for sugar (fructose) as a cause of obesity in the American Journal of Clinical Nutrition a few years ago. [1]
What the animal studies show us is that when fructose and vegetable oils are consumed together, they multiply each other’s obesity-inducing effects.
Consistent with this, the obesity explosion in the UK and US is accompanied with dramatic increases (+200% or more) in both polyunsaturated fat and sugar (which is half fructose; roughly the same as high-fructose corn syrup, really).
PUFA (in many vegetable oils) is generally bad even though EPA+DHA are good. Omega-6 PUFA intake is generally too high in our diet already. When you’re losing fat weight, you’ll have a lot of omega-6 in your bloodstream assuming you had a normal diet when you put it on, so that means you’d want even less omega-6 in your diet and more omega-3.In the China Study, the correlation of wheat consumption with BMI was 56%, whereas the correlation of total calorie intake with BMI was only 13%. (Since total calorie intake is correlated with muscle mass, total calorie intake may be completely uncorrelated with fat mass. It’s not how much you eat, but how much wheat!)
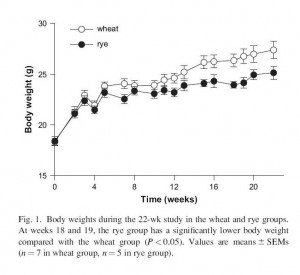
Similar outcomes occur in mice. I can’t find any mouse studies comparing wheat to rice, but I did find one comparing wheat to rye [4]. Wheat was far more obesity-inducing than rye:
Since rye has gluten, it’s not just the gluten in wheat causing obesity (many people vilify gluten, but other than for a minority of people with celiac disease, it’s not clear what the problem with it is).
Dietary glucose is not likely to do much damage unless the body’s glucose-disposal machinery has been damaged by other toxins first.
(fructose is a toxin; something in wheat is a toxin); but fructose in a low-carb diet may go straight to glycogen (especially if it’s after exercise which drains your muscles’ glycogen stores), which is safe. fructose+saturated fat is safer than fructose+PUFA as mentioned above (thank goodness for all that saturated fat in my oversweetened ice cream!)
It’s possible, by the way, that differing toxicities among grains could be responsible for epidemiological evidence favoring “whole grains” over “refined grains.” In America, products made with refined grains are usually 100% wheat; but products made with whole grains are often of mixed origin (“7 grain bread”). Since wheat is the most obesity-inducing grain, dilution of wheat content may be masking the toxicity of whole grains.
I also eat bananas and stone fruits and tend to avoid apples and pears.
(apple+pear are essentially fructose+fiber. fiber may slightly reduce the harm from fructose, but it’s still bad)
Beans have a lot of toxins in their raw state. They can sometimes be detoxified by overnight soaking and thorough cooking. With commercial products we don’t really know what they did to process the beans.
I really do think commercial beans are soaked and cooked.